If patient PREGNANT, contact obstetric team
DEFINITION
Deep vein thrombosis (DVT) is the development of a thrombus (blood clot) that completely or partially occludes a deep vein, usually in the legs
RECOGNITION
Symptoms and signs
- Swelling of limb (arm, calf or leg)
- measure circumference 10 cm below tibial tuberosity and compare with asymptomatic limb
- difference of >3 cm increases probability of DVT
- Pain and stiffness of affected limb
- Pitting oedema
- Increased skin temperature
- Erythema
- Tenderness
- Mild fever
Pregnancy
- It can be difficult to distinguish symptoms and signs of DVT from normal pregnancy
- exercise vigilance in pregnant woman – discuss with obstetric registrar/specialist trainee
Complications
- In rare cases, arterial circulation may be severely compromised:
- severe pain, swelling, cyanosis
- rapid development of tense blue oedema (phlegmasia cerulea dolens)
- If patient is an injection drug user, examine for:
- localised infection e.g. erythema or fluctuance suggesting infected clot
- deep soft tissue infection, abscess at injection site
- necrotising fasciitis
- acute arterial occlusion, and/or myositis
- systemic infection and septic embolic abscesses e.g. cardiac murmurs suggesting infective endocarditis, sepsis, haemoptysis and cough with purulent sputum
Differential diagnosis
- Ruptured Baker’s cyst
- history of arthritis or trauma to knee
- swelling behind knee
- examine for arthropathy and effusion
- Torn calf muscles/damage to Achilles tendon
- sudden pain in calf following twisting of leg
- examine for haematoma
- disruption of tendon indicates severe rupture
- Cellulitis – see Cellulitis guideline
- Fracture
- Oedema (heart failure, hypoalbuminemia, lymphatic obstruction, dependant)
- Acute Charcot arthropathy
- consider if longstanding diabetic with peripheral neuropathy and/or history of trauma
- advise reducing weight bearing
- refer urgently to diabetic nurse, podiatry and orthopaedics
INVESTIGATIONS
- FBC, INR, APTT, LFTs, and U&E
- If patient is an injection drug user or has signs of infection:
- CRP
- blood cultures
- chest X-ray (to exclude septic embolic lung abscesses)
- ultrasound of groin area (localised collection)
- echo if murmur, positive blood cultures or chest X-ray suggestive of septic embolic lung abscesses
- offer testing for blood borne viruses (HIV, HBV, HCV) – see HIV infection testing guideline
D-dimer
- Raised in many clinical states. See Common causes of raised D-dimer concentration
- normal D-dimer concentration virtually rules out thrombosis
Common causes of raised D-dimer concentration
- Acute myocardial infarction (MI)
- Chronic subdural haematoma
- Disseminated intravascular coagulation
- Gram-negative bacteraemia
- Leukaemia
- Liver disease
- Metastatic malignancy
- Peripheral vascular disease
- Pregnancy
- Recent surgery
- Renal disease
- Rheumatoid disease
- Sickle cell crisis
- Subarachnoid haemorrhage
- Thrombolytic therapy
- Trauma with pathological thrombosis
ASSESSMENT
- If DVT suspected in a woman who is pregnant or has given birth within the last 6 weeks:
- Do not use two-level DVT Wells score
- immediately commence dalteparin. See Dalteparin for VTE guideline
- refer immediately for same-day Doppler scan
- discuss with obstetrics registrar/specialist trainee
Doppler scan negative
- If low clinical suspicion of DVT, discontinue treatment
- If DVT clinically likely, continue treatment and repeat Doppler scan in 6–8 days
- if positive, continue treatment
- if negative, discuss other imaging modalities with radiologist and obstetric consultant
Doppler scan positive
- Discuss with obstetric registrar or specialist trainee
- Commence/continue treatment for DVT
Calculate two-level DVT Wells score using tool
Table 1: Two-level DVT Wells score
| Clinical feature | Points |
| Paralysis, paresis or recent plaster immobilisation of lower extremities | 1 |
| Recently bedridden for ≥3 days or major surgery within 12 weeks requiring general or regional anaesthesia | 1 |
| Localised tenderness along distribution of deep venous system | 1 |
| Entire leg swollen | 1 |
| Calf swelling at least 3 cm larger than asymptomatic side. Measure circumference 10 cm below tibial tuberosity | 1 |
| Pitting oedema confined to symptomatic leg | 1 |
| Malignancy (on treatment, treated in last 6 months or palliative) | 1 |
| Collateral superficial veins (non-varicose) | 1 |
| Previously documented DVT | 1 |
| An alternative diagnosis is at least as likely as DVT | -2 |
| Clinical probability simplified score | |
| DVT likely | ≥2 points |
| DVT unlikely | ≤1 point |
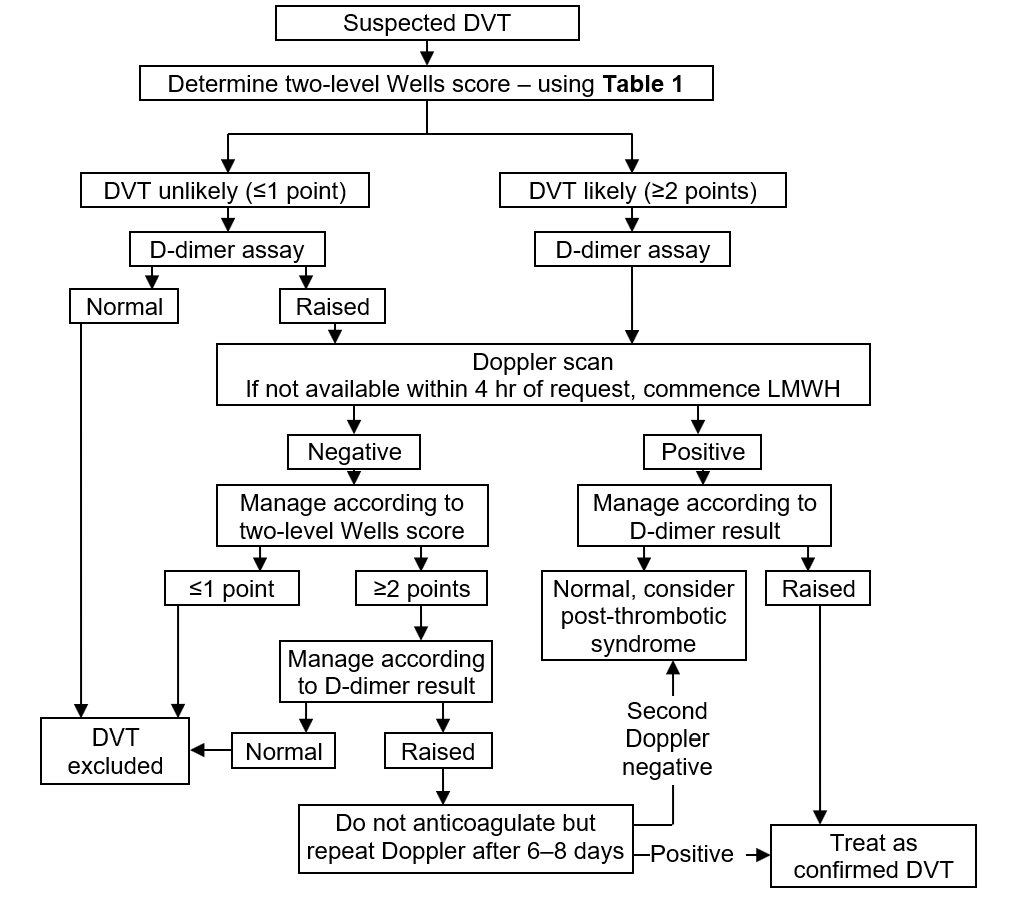
Flowchart for DVT management
D-dimer result available
- Select calculated two-level DVT Wells Score and D-dimer combination
Doppler scan indicated
- Local booking instructions
- If Doppler ultrasound scan cannot be arranged within 4 hr of request, but patient can otherwise be discharged:
- start SC dalteparin (see Dalteparin for VTE guideline) or direct oral anticoagulants (see DOAC in VTE guideline)
- if delay >24 hr (e.g. bank holiday), follow local instructions
Doppler and D-dimer results available
Select correct Doppler result, DVT Wells Score and D-dimer combination - see Flowchart for DVT management
MANAGEMENT
- Encourage ambulation
- Elevation of leg when seated
- Simple analgesia (e.g. paracetamol or if inadequate control, co-codamol)
- Discuss with obstetric registrar/specialist trainee
- Dalteparin and warfarin are not contraindicated in breastfeeding
- Either continue dalteparin (see Dalteparin for VTE guideline) for 8–12 weeks followed by prophylactic dose for the rest of pregnancy and ≥6 weeks postnatally. See Prophylaxis against venous thromboembolism guideline
- Or if woman chooses to commence warfarin to complete anticoagulation treatment postpartum, avoid until third postnatal day. See Warfarin initiation guideline
- If anticoagulation contraindicated, consultant physician, staff physician must decide which carries most risk – complications of therapy (consider vena caval filter) or DVT/PE
Inferior vena caval filter (IVCF)
- IVC filters carry significant morbidity and mortality risks and only be offered if:
- anticoagulation treatment contraindicated in confirmed proximal DVT or PE. Remove IVCF when anticoagulation treatment
- no longer contraindicated and has been established
- person with proximal DVT or PE has a PE while taking anticoagulation
- Discuss with haematologist before requesting IVCF treatment only
- Before fitting an IVCF, ensure there is a strategy in place and documented for removal at earliest possible opportunity
Choice of anticoagulation long-term
Warfarin preferred if:
- History of antiphospholipid syndrome
- Interacting medication
- Concurrent metallic heart valve
- Recurrent thrombosis whilst therapeutically anticoagulated
LMWH therapy for duration of treatment preferred if:
- Injection drug user
- Active cancer, particularly luminal GI and GU neoplasms
- At risk of GI bleeding
- If continuing with dalteparin, inform local anticoagulation service
Start of anticoagulation
- Start as soon as PE suspected
- If aiming to continue anticoagulation long-term with dalteparin, warfarin, edoxaban or dabigatran, commence dalteparin - see Dalteparin for VTE and DOAC for VTE guidelines
- If aiming to continue anticoagulation long-term with apixaban or rivaroxaban, start DOAC immediately - see DOAC for VTE guideline
DVT confirmed
- Start chosen long-term anticoagulant
- if continuing anticoagulation with warfarin, edoxaban or dabigatran, continue dalteparin (see Dalteparin for VTE guideline) for minimum of 5 days
- For details of drugs see DOAC in VTE guideline or Warfarin initiation guideline
COMPLICATIONS
Suspected phlegmasia cerulea dolens (painful blue oedema)
- An uncommon manifestation of massive DVT compromising venous outflow and causing ischemia and manifesting as a painfully swollen blue leg
- Elevate bed foot to 40° and ensure fluid replacement adequate to compensate for extravasation
- Refer urgently to on-call general surgical team
Concomitant infection
- Treat cellulitis or sepsis – see Cellulitis guideline and Sepsis guideline
- If evidence of groin abscess, refer to on-call surgical team
- If evidence of septic pulmonary embolism on chest X-ray, admit to respiratory or infectious diseases ward
Symptomatic ileo-femoral DVT
- Suggested by back pain and swelling of entire limb
- Discuss with radiologist (and if pregnant, obstetrician) to consider magnetic resonance venography
Treatment
- Consider catheter guided thrombolysis or mechanical thrombectomy if:
- symptoms of <14 days duration
- good functional status
- life expectancy of ≥1 yr
- low risk of bleeding (for thrombolysis)
- Discuss with interventional radiologist and vascular surgeon
- Do not prescribe elastic graduated compression stockings to prevent post-thrombotic syndrome or VTE recurrence after a proximal DVT
SCREENING
- If no clear precipitating cause for thrombosis, particularly if this is a recurrent event, consider occult malignancy or other cause of thrombophilia
- If patient aged <45 yr with unprovoked DVT, discuss screening for inherited or acquired thrombophilia with haematology consultant
Screen for cancer
- In all patients with confirmed DVT, chest X-ray, FBC, LFT, calcium and urinalysis
- Only offer further investigations for cancer to people with unprovoked DVT if they have relevant symptoms or signs
DISCHARGE
Outpatient
- Unless symptoms severe, or patient an injection drug user, or requires admission to hospital for reasons other than suspected DVT, treat as outpatient
- ensure form authorising daily injections of dalteparin completed once diagnosis confirmed
Duration of treatment
- Treatment will be continued for 3 months, but duration may be longer if DVT was unprovoked, recurrent or in the presence of cancer or non-modifiable risk factor such as significant immobility
Advice to patient
- Many drugs (including alcohol) interact with warfarin or DOAC
- To remind their GP, if additional medication is added, that they are taking anticoagulant
- To inform dentist that they are anticoagulated
- Give advice on extended travel
- Provide PE information booklet
Women of childbearing age (Pregnancy, Pills, Periods)
- Counsel that DOACs and warfarin may be harmful in pregnancy.
- seek immediate advice if pregnant or trying to conceive
- Anticoagulation may lead to menorrhagia in 70% of women. Apixaban less commonly implicated than warfarin and rivaroxaban
- Do not stop contraception at time of PE diagnosis including combined oral contraceptive pill (COCP)
- Refer patient to thrombosis clinic to discuss options
- Anticoagulation negates the ongoing thrombotic risk of the COCP. Stopping COCP may precipitate menorrhagia or lead to pregnancy whilst on a DOAC
Monitoring of warfarin
- Refer to anticoagulant management service for follow-up appointment date
- Give patient a completed yellow anticoagulation therapy record - see Warfarin for VTE guideline
- Ensure discharge letter includes diagnosis, dosage of warfarin and date of clinic appointment
- If anticoagulation to be monitored by GP, supply GP with written information (on separate sheet, stapled to discharge letter) about:
- indication for anticoagulation
- proposed duration of treatment
- proposed target range for INR
- details of anticoagulation in hospital (give dates, INR results and dosage taken)
Document
- Document in medical record
- patient has been given written and verbal information about warfarin and has been referred to anticoagulation clinic
- duration of treatment
- if definite risk factor identified
- outpatient investigations
- monitoring arrangements
Follow-up
- Arrange appointment in 10-12 weeks for appropriate medical clinic
- unless a shorter course of treatment or need for investigation requires earlier follow-up; patients with confirmed DVT remain under the care of duty physician for the day on which diagnosis was confirmed
- send copy of letter to patient’s GP
FOLLOW-UP CLINIC
- If patient has active cancer, reassess risks and benefits of continuing anticoagulation at 6 months
- After a first proximal DVT without a clear underlying cause or if permanent risk factors present, assess VTE risk and discuss with patient, if anticoagulation should be continued
Last reviewed: 2025-06-19