DEFINITION
- Pneumonia that is acquired outside hospital and includes pneumonia that develops in a nursing home
RECOGNITION AND ASSESSMENT
- If patient has symptoms and signs below plus new unexplained chest X-ray shadowing, and the illness is the primary clinical problem, treat as pneumonia
Symptoms
- Malaise, fever, rigors
- Vomiting, diarrhoea
- Confusion (especially in the elderly)
- Dyspnoea, cough
- Sputum (may be blood-stained, viscid and difficult to expectorate)
- Pleuritic pain
Social history
- Enquire about
- pet birds (psittacosis, chlamydial infection)
- recent hotel residence away from home (legionellosis)
Signs
- High fever (often absent in the elderly, where hypothermia may be seen)
- Tachycardia
- Tachypnoea
- Localised crackles
- Bronchial breathing (in about one third of hospital admissions)
- Chest signs may be absent or masked by other respiratory signs (e.g. COPD, CCF)
- Check for signs of immunosuppression - e.g. oral candidiasis
Investigations
- Chest X-ray
- within 4 hr of arrival at hospital
- Oximetry
- if SpO2 <94% or features of severe pneumonia (see severity assessment below), measure arterial blood gas (ABG)
- FBC, U&E, LFT, CRP
- Microbiology:
- include full clinical history on request
- sputum - culture and sensitivity
- in moderate or severe severity send sputum for mycoplasma PCR
- blood cultures in all patients requiring IV antibiotics, irrespective of temperature - see Blood culture guideline
- in moderate or severe severity perform nose and throat swab in viral transport media for atypical organisms (influenza A and B, Chlamydia psittaci, Coxiella burnetii, Mycoplasma pneumoniae, Legionella pneumophila). Indicate date of onset clearly on request form
- in moderate or severe severity send urine for legionella antigen and pneumococcal antigen
- if available, perform point of care test for respiratory pathogens
Differential diagnosis
- Pulmonary thromboembolism
- Lung cancer
- Left ventricular failure
IMMEDIATE MANAGEMENT
Severity
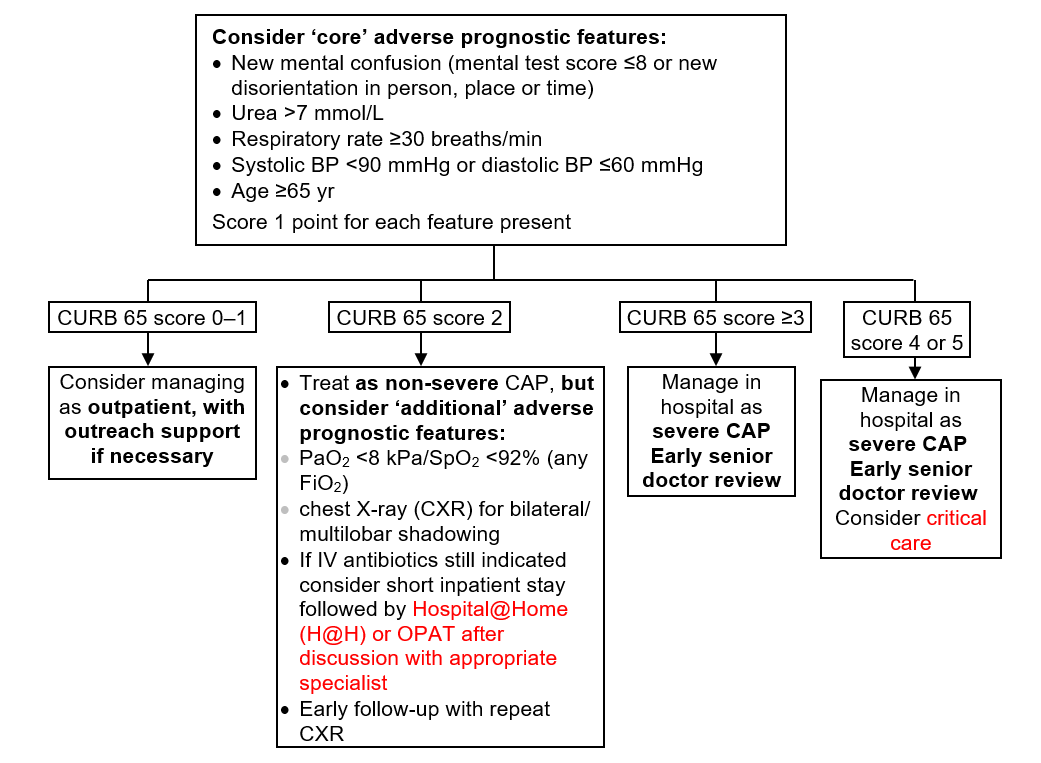
- Management is based on the CURB 65 assessment of severity
CURB 65 assessment
Acute necrotising pneumonia
- If a previously healthy young adult presents with acute necrotising pneumonia with rapid lung cavitation, suspect Panton-Valentine Leukocidin (PVL) toxin-producing Staphylococcus aureus
- isolate in single room and contact microbiologist, infectious disease, or respiratory consultant
Admission
- Admit to a respiratory ward
- if patient meets the frail elderly criteria and has pneumonia as well as other diagnoses, consider admission to elderly care ward
Supportive therapy
- Oxygen if SpO2 <94%. See Hypoxaemia guideline
- Fluid replacement to compensate for effects of pyrexia and tachypnoea coupled with inadequate intake. See Fluid management guideline
- Prophylactic LMWH
- Treat any accompanying airflow obstruction or cardiac failure
- Physiotherapy only in patients with copious secretions
Analgesia for pleuritic pain
- Paracetamol alone is unlikely to be adequate
- If patient on ACE inhibitor or pregnant, avoid NSAIDs
- prefer morphine sulphate 10 mg oral 4-hrly
- If well hydrated and eGFR ≥30 mL/min, ibuprofen 400 mg oral 8-hrly
- In dehydrated patient or if eGFR <30 mL/min, to prevent renal damage, prefer morphine sulphate 10 mg oral 4-hrly
- if eGFR ≥30 mL/min, ibuprofen may be substituted once adequate fluid replacement achieved
Antimicrobial therapy
- Start as soon as diagnosis made - give first dose within 1 hr of presentation to hospital and before leaving assessment area
- therapy should always cover Streptococcus pneumoniae
- Route of administration depends whether patient able to swallow and absorb oral drugs, severity of illness and likely pathogens
- See current BNF for interactions
- e.g. statins contraindicated in combination with clarithromycin
- avoid doxycycline in pregnancy
Penicillin Allergy
- True penicillin allergy is rare
- Ask the patient and record what happened when they were given penicillin
- If any doubt about whether patient is truly allergic to penicillin, seek advice from a microbiologist or consultant in infectious diseases
Infection Control alerts
- Check IC alert
- if IC alert not available, check previous 12 months of microbiology reports
- if MRSA present, treat as tagged for MRSA. See MRSA management
- if ESBL, MGNB, CARB present, treat as tagged for ESBL. See ESBL/MGNB/CARB management
Choice of Antimicrobials
- Statins contraindicated in combination with clarithromycin (see current BNF for other interactions)
Aspiration results in chemical pneumonitis which may result in increased inflammatory markers. Pneumonia secondary to aspiration develops only in a proportion of these patients generally after several hours to days. Establish that there is evidence of pneumonia before starting antimicrobial therapy
First line
- Metronidazole 500 mg IV by infusion or 400 mg oral 8-hrly plus amoxicillin 1 g IV/ oral 8-hrly
- switch to oral as soon as possible
- If MRSA tagged in iPortal: Add vancomycin IV by infusion - see Vancomycin guideline and Vancomycin calculator
Alternative (penicillin allergy)
- Metronidazole 500 mg IV by infusion or 400 mg oral 8 hrly plus levofloxacin 500 mg IV by infusion/ oral daily
- switch to oral as soon as possible
- In patients at high risk of Clostridium difficile associated colitis, discuss with consultant microbiologist/ID
- If MRSA tagged in iPortal: Add vancomycin IV by infusion - see Vancomycin guideline and Vancomycin calculator
Aspiration results in chemical pneumonitis which may result in increased inflammatory markers. Pneumonia secondary to aspiration develops only in a proportion of these patients generally after several hours to days. Establish that there is evidence of pneumonia before starting antimicrobial therapy
First line
- Co-amoxiclav 1.2 g IV 8-hrly
- If treating Immunocompromised patient, patient with previous respiratory samples growing in the previous 12 months Pseudomonas aeruginosa or organisms resistant to co-amoxiclav, piperacillin/tazobactam 4.5 g IV 8-hrly
- If MRSA tagged in iPortal: Add vancomycin IV by infusion - see Vancomycin guideline and Vancomycin calculator
Alternative (penicillin allergy)
- Co-trimoxazole 960 mg IV/NG 12-hrly (contains trimethoprim) plus metronidazole 500 mg IV by infusion or 400 mg oral 8-hrly
- If MRSA tagged in iPortal: Add Vancomycin IV by infusion - see Vancomycin guideline and Vancomycin calculator
- Isolate in single room and contact microbiologist, infectious diseases or respiratory consultant for advice
First line
- Clindamycin 1.2 g IV infusion 6-hrly plus
- Rifampicin 600 mg IV infusion 12-hrly plus
- Linezolid 600 mg IV infusion 12-hrly plus
- Co-amoxiclav 1.2 g IV 8-hrly
Alternative (penicillin allergy)
- Substitute co-amoxiclav with levofloxacin 500 mg IV by infusion 12-hrly
- in patients at high risk of Clostridium difficile associated colitis, discuss with consultant microbiologist/ID
Other treatment
- Consider IVIG at an early stage and discuss with consultant microbiology or consultant in infectious diseases
Duration: 14 days minimum
Treat Staphylococcal pneumonia aggressively, but do not treat every Staphylococcus aureus isolated in sputum as this commonly represents oropharyngeal colonisation
First line
- Flucloxacillin 2 g IV 6-hrly
- if severe/necrotising pneumonia, see Necrotising pneumonia above
Alternative (penicillin allergy)
Vancomycin IV by infusion (see Vancomycin guideline and Vancomycin calculator)
IV should be transferred to oral as soon as clinical improvement occurs and temperature has been normal for 24 hr, providing there is no contraindication to oral therapy and a suitable agent is available
Duration: 14 days total (including IV treatment)
Not severe: doxycycline (avoid in pregnancy) 100 mg oral 12-hrly
Severe: clarithromycin 500 mg IV by infusion 12-hrly
IV should be transferred to oral as soon as clinical improvement occurs and temperature has been normal for 24 hr, providing there is no contraindication to oral therapy
Not severe: Clarithromycin 500 mg oral 12-hrly
Severe: Levofloxacin 500 mg IV by infusion 12-hrly. In patients at high risk of Clostridium difficile associated colitis, discuss with consultant microbiologist/ID
IV should be transferred to oral as soon as clinical improvement occurs and the temperature has been normal for 24 hr, providing there is no contraindication to oral therapy
Duration
Not severe: 14 days total (including IV treatment)
Severe: 14-21 days total (including IV treatment)
Perform HIV screen
First line
- Amoxicillin 1 g oral 8-hrly
- if no NG/PEG tube and unable to swallow or absorb oral drugs: Benzylpenicillin 1.2 g IV 4-hrly
Alternative (penicillin allergy)
- If Pneumococcus sensitive: Clarithromycin 500 mg oral 12-hrly
- if no NG/PEG tube and unable to swallow or absorb oral drugs: clarithromycin 500 mg IV by infusion 12-hrly
- If not sensitive to clarithromycin, discuss with consultant in infectious diseases or microbiologist
- For patients admitted to critical care facility: Add vancomycin IV by infusion - see Vancomycin guideline and Vancomycin calculator
- Send rectum swab (and CSU if long-term catheter) for ESBL screen
- Contact microbiology for advice
If patient tagged for MRSA in iPortal
Add vancomycin IV by infusion - see Vancomycin guideline and Vancomycin calculator
First line
- Co-amoxiclav 1.2 g IV 8-hrly plus
- Doxycycline (avoid in pregnancy) 100 mg oral 12-hrly
- if nil-by-mouth, replace doxycycline with clarithromycin 500 mg IV by infusion into larger proximal vein 12-hrly
- If legionella suspected: levofloxacin 500 mg oral/IV by infusion 12-hrly alone
- in patients at high risk of Clostridium difficile associated colitis, discuss with consultant microbiologist/ID
- If Staphylococcal pneumonia or necrotising pneumonia suspected: see separate guidelines
Alternative (penicillin allergy)
- Discuss with respiratory consultant or consultant microbiologist/infectious diseases
- Levofloxacin 500 mg IV by infusion 12-hrly
- in patients at high risk of Clostridium difficile associated colitis, discuss with consultant microbiologist/ID
- For patients admitted to critical care facility add vancomycin IV by infusion - see Vancomycin guideline and Vancomycin calculator
- Oral stepdown: levofloxacin 500 mg oral 12-hrly
If patient tagged for MRSA in iPortal
- Add vancomycin IV by infusion - see Vancomycin guideline and Vancomycin calculator
- IV only needed if no NG/PEG and unable to swallow or absorb oral drugs. Convert to oral route as soon as available
- If not responding within 24-48 hr, treat as severe pneumonia and repeat CXR
First line
- Amoxicillin 1 g oral 8-hrly plus doxycycline (avoid in pregnancy) 100 mg oral 12-hrly
- If legionella suspected: amoxicillin 1 g oral 8-hrly plus clarithromycin 500 mg oral 12-hrly
- If IV needed: amoxicillin 1 g IV 8-hrly plus clarithromycin 500 mg IV by infusion into larger proximal vein 12-hrly
Alternative (penicillin allergy)
- Doxycycline (avoid in pregnancy) 100 mg oral 12-hrly
- If IV needed: clarithromycin 500 mg IV by infusion into larger proximal vein 12-hrly
If patient tagged for MRSA in iPortal
- Add vancomycin IV by infusion - see Vancomycin guideline and Vancomycin calculator
- Add vancomycin IV by infusion - see Vancomycin guideline and Vancomycin calculator
First line
- Amoxicillin 500 mg oral 8-hrly
Alternative (penicillin allergy)
- Doxycycline 200 mg oral once daily for 1 day then 100 mg once daily - avoid in pregnancy
Assessment of requirement for intensive care
- Indications for transfer to critical care include:
- severe pneumonia on CURB 65 score (4 or 5)
- arterial PaO2 ≤8 kPa with inspired oxygen ≥60%
- severe acidosis - pH <7.25
- exhausted, drowsy or unconscious patient
- respiratory or cardiac arrest
- shock
- ensure treatment escalation plan in place - discuss with patient and family
MONITORING TREATMENT
- In severe pneumonia, clinical assessment (including mental state) 12-hrly, until improving
- Pulse, BP, temperature, respiratory rate and SpO2 with FiO2 4-hrly until stable
- aim for SpO2 ≥92%
- if type 2 respiratory failure - see Respiratory failure guideline
- Biochemical screen - repeat every 24-48 hr while significant abnormalities persist
- If patient not improving after 48 hr despite adequate therapy, repeat chest X-ray and CRP
- if CRP not falling, consider possibility of empyema, abscess or inappropriate antimicrobial regimen
SUBSEQUENT MANAGEMENT
- Nutritional support in prolonged illness
- If risk factors for HIV are present or recurrent pneumonia, test for HIV - see HIV infection testing guideline
Duration of antimicrobials
- If IV route used on admission, change to oral when clinical improvement occurs and temperature normal for 24 hr
- use oral antimicrobial to which microbe sensitive
- If sensitivity not known, give co-amoxiclav 625 mg oral 8-hrly plus doxycycline 100 mg (avoid in pregnancy) oral 12-hrly. If allergic to penicillin, levofloxacin 500 mg oral 12-hrly
- In uncomplicated pneumonia non-severe, give 3-5 days treatment including IV treatment
- In patients with severe pneumonia, necrotising pneumonia, staphylococcal pneumonia, or legionella pneumonia, continue antimicrobials for at least 7-10 days including IV treatment
Failure to respond to therapy
- Request review by specialist in respiratory medicine/infectious disease and consider:
- incorrect diagnosis (e.g. pulmonary embolism, pulmonary oedema, pulmonary eosinophilia, Wegener's granulomatosis)
- resistant organism (e.g. amoxicillin-resistant/penicillin-resistant Strep. pneumoniae, haemophilus, mycoplasma, psittacosis, Q fever or staphylococcal pneumonia) - discuss with microbiologist
- unrecognised pulmonary tuberculosis
- unrecognised immunodeficiency (e.g. HIV infection leading to pneumocystis pneumonia)
- Complications:
- parapneumonic effusion or empyema - aspirate, culture and drain, and refer to respiratory physician - see Pleural infection and empyema guideline
- lung abscess - refer to respiratory physician
- bronchial obstruction - refer to respiratory physician
- pulmonary embolism - see Pulmonary embolism guidelines
- fever related to drug therapy - omit therapy for 48 hr
DISCHARGE AND FOLLOW-UP
- Check within 24 hr of planned discharge that patient does not have more than one of the following:
- temperature >37.8°C
- heart rate >100/min
- respiratory rate >24/min
- systolic blood pressure <90 mmHg
- oxygen saturation <90%
- inability to maintain oral intake
- abnormal mental status
- Clinical review by GP or in hospital clinic after approximately 6 weeks
- request follow-up Chest X-ray before patient discharged for all patients who have persistent symptoms or are at high risk of underlying malignancy (especially smokers and those aged >50 yr) whether or not they have been admitted
- convalescent serology can be obtained at this visit
- Record smoking status and offer smoking cessation advice if appropriate
- Provide written information about pneumonia, available at - https://bestpractice.bmj.com/patient-leaflets/en-gb/html/1585255253371/Pneumonia