- If the patient is pregnant, contact obstetric team
DEFINITION
- Haemodynamically stable pulmonary embolism (PE) with systolic BP ≥90 mmHg and <40 mmHg drop from baseline
- PE range from small with normal BP to large with borderline BP and right ventricular dysfunction
- If patient becomes haemodynamically unstable during management, follow Pulmonary embolism: Haemodynamically unstable guideline
RECOGNITION
- Pulmonary venous thromboembolism (PE) is often missed clinically, particularly in:
- severe cardiorespiratory disease
- elderly patients
- Suspect the diagnosis in any patient who does not respond to initial therapy, or in whose condition there has been an unexplained deterioration
- Most episodes follow popliteal or iliofemoral DVT
Symptoms
- Small emboli present with dyspnoea
- Moderate-sized emboli present with signs of infarction and pleuritic pain
- Dyspnoea (present in 90% of cases) - may be of sudden onset
- Pleuritic chest pain
- Haemoptysis
- Syncope
Signs
- Tachypnoea (>20 breaths/min)
- Fever
- Pleural rub
- Tachycardia
- Maybe absent
Differential diagnosis
- Pneumonia
- Myocardial infarction (MI)
- Exacerbations of asthma and COPD
INITIAL ASSESSMENT
Pulmonary embolism rule-out criteria (PERC)
- If clinical suspicion of PE is low (the clinician estimates <15% probability and other diagnoses are feasible), assess PERC to help determine whether any further investigations for PE are needed
- If patient has any of the following criteria, a D-dimer and two-level PE Wells score would be required, and follow flowchart below
- aged ≥50 yr
- heart rate ≥100 bpm
- oxygen saturation on air <95%
- unilateral leg swelling
- haemoptysis
- recent surgery or trauma ≤4 weeks ago and requiring a general anaesthetic
- hormone use - oral contraceptive pill, HRT, oestrogen therapy in man or woman
- previous PE or DVT
- If patient has none of the above criteria, chance of PE is <2%
INVESTIGATIONS
- FBC, INR, APTT and U&E
ECG and CXR
- ECG and CXR (with fetal screening in a pregnant woman) are often normal
- not to be used to confirm/refute the diagnosis
- useful for identifying other diseases and explaining symptoms
- ECG may show:
- sinus tachycardia, an S1 Q3 T3 pattern
- right bundle branch block, P pulmonale or right axis deviation
- Chest X-ray may show:
- non-specific shadows or a raised hemidiaphragm
- pulmonary oligaemia, linear atelectasis or small pleural effusion
D-dimer
- Raised in many clinical states
- do not request if clinical probability of PE is high, in probable massive and haemodynamically unstable PE, or where an alternative diagnosis is highly likely
- normal D-dimer concentration virtually rules out thrombosis
Leg Doppler ultrasound
- Alternative to lung imaging in patients with clinical DVT
CTPA
- Gold standard
- often shows other diagnoses
- for patients with contrast media allergy, severe renal impairment (eGFR <30 mL/min) or at high risk from radiation, assess most appropriate imaging modality with radiologist
ASSESSMENT
- If PE suspected in a woman who is pregnant or has given birth within the last 6 weeks:
- refer to obstetric guidelines
- refer immediately for same-day Doppler scan
- discuss with obstetrics registrar/specialist trainee
- if Doppler scan negative discuss with radiologist preferred imaging modality – ventilation perfusion scan (V/Q), CTPA or V/Q planer scan
- Order test indicated by two-level PE Wells score, clinical status and CXR result
Table 2: Two-level PE Wells score
| Clinical feature | Points |
|
Symptoms and signs of DVT |
3 |
| An alternative diagnosis is less likely than PE | 3 |
| Heart rate >100 beats/min | 1.5 |
| Immobile for >3 days or surgery in previous 4 weeks | 1.5 |
| Previous DVT or PE | 1.5 |
| Haemoptysis | 1 |
| Malignancy (currently being treated, treated in last 6 months, or palliative) | 1 |
| Clinical probability simplified score | |
| PE likely | >4 points |
| PE unlikely | ≤4 points |
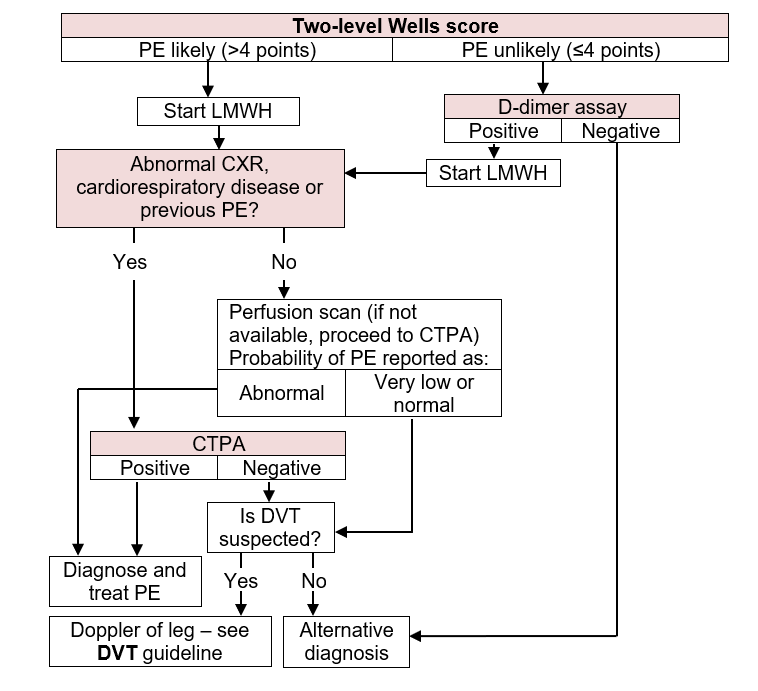
Flowchart for diagnosis of non-massive PE
CTPA selected
Positive for PE
- PE confirmed. Treat
Negative for PE
- If DVT suspected, order doppler of leg. See Deep vein thrombosis (DVT) guideline
- If DVT not suspected, consider alternative diagnosis
D-dimer selected
D-dimer result raised
- Start LMWH. See Enoxaparin for VTE guideline
- Order CTPA
D-dimer result not raised
- Consider alternative diagnosis
SUPPORTIVE MANAGEMENT
General
- Oxygen - see Hypoxaemia guideline
- Adequate analgesia for pleuritic pain - paracetamol alone is unlikely to be adequate
- if well hydrated and eGFR ≥30 mL/min, ibuprofen 400 mg oral 8-hrly
- in dehydrated patient or if eGFR <30 mL/min, to prevent renal damage, prefer morphine sulphate 10 mg oral 4-hrly - ibuprofen may be substituted once adequate fluid replacement achieved if eGFR ≥30 mL/min
- if patient pregnant, prefer morphine sulphate 10 mg oral 4-hrly
- if patient taking ACE inhibitor avoid NSAIDS, including ibuprofen
- A high right atrial pressure (i.e. ↑JVP) is common and does not need to be treated
- AVOID diuretics
When to use protein pump inhibitor (PPI)
- Concurrent antiplatelet therapy doubles the risk of major bleeding with anticoagulation
- confirm safety of stopping with specialist teams (i.e. cardiology, neurology)
- if antiplatelet therapy must continue, recommend PPI
- SSRI and SNRI medications also increase the risk of GI bleeding with anticoagulation
- recommend PPI to mitigate this risk
Management of confirmed VTE
Discuss with obstetric registrar/specialist trainee
- Enoxaparin and warfarin are not contraindicated in breastfeeding
- Either continue enoxaparin (see obstetric guidelines and Enoxaparin for VTE guideline) for 8-12 weeks followed by prophylactic dose for the rest of pregnancy and ≥6 weeks postnatally. See obstetric guideline for prophylaxis
- Or if woman chooses to commence warfarin to complete anticoagulation treatment postpartum, avoid until third postnatal day. See Warfarin initiation guideline
If anticoagulation contraindicated, consultant physician or staff physician must decide which carries most risk - complications of therapy (consider a vena caval filter) or the DVT/PE
Inferior vena caval filter (IVCF)
- IVC filters carry significant morbidity and mortality risks and should only be offered if:
- anticoagulation treatment is contraindicated in confirmed proximal DVT or PE. Remove IVCF when anticoagulation
- treatment is no longer contraindicated and has been established
person with proximal DVT or PE has a PE while taking anticoagulation
- Discuss with haematologist before requesting IVCF treatment only
- Before fitting an IVCF, ensure that there is a strategy in place and documented for it to be removed at the earliest possible opportunity
Choice of anticoagulation for required duration of treatment
DOAC
- Use DOAC unless alternative anticoagulation is indicated – see below
Warfarin preferred if:
- History of anti-phospholipid syndrome
- Interacting medication
- Concurrent metallic heart valve
- Recurrent thrombosis whilst therapeutically anticoagulated
LMWH therapy for duration of treatment preferred if:
- Injection drug user
- Active cancer, particularly luminal GI and GU neoplasms
- At risk of GI bleeding
- If continuing with enoxaparin, inform local anticoagulation service
Start of anticoagulation
- Start as soon as PE suspected
- If aiming to continue anticoagulation for required duration with enoxaparin, warfarin, edoxaban or dabigatran, commence enoxaparin- see Enoxaparin for VTE and Direct oral anticoagulant (DOAC) for venous thromboembolism (VTE) guidelines
- If aiming to continue anticoagulation for required duration with apixaban or rivaroxaban, start these DOAC immediately see Direct oral anticoagulant (DOAC) for venous thromboembolism (VTE) guideline
PE or DVT confirmed
- Start chosen long-term anticoagulant
- if continuing anticoagulation with warfarin, edoxaban or dabigatran. continue enoxaparin (see Enoxaparin for VTE guideline) for a minimum of 5 days
- For details of drugs see DOAC in VTE guideline or Warfarin initiation guideline
ASSESS SUITABILITY FOR AMBULATORY CARE
- Assess patients by sPESI risk score and exclusion criteria
Determine Simplified Pulmonary Embolism Severity Index (sPESI)
Table 3
| Parameter | Score |
| Age >80 yr | 1 |
| Active cancer (diagnosed within 12 months or undergoing treatment) | 1 |
| Chronic cardiopulmonary disease | 1 |
| Pulse ≥110 bpm | 1 |
| Systolic blood pressure <100 mmHg | 1 |
| Oxygen saturation ≤90% (with or without supplemental oxygen) | 1 |
| Risk Class | |
| Low | 0 |
| High | ≥1 |
Check exclusion criteria
Decision
- If sPESI is high risk or an exclusion criterion, manage as inpatient
- consider for early discharge when low risk score
- If SPESI is low risk and no exclusion criterion, manage as ambulatory care
Suitable for ambulatory care of PE
- Refer to ambulatory emergency care centre (AEC)
- Provide patient information on:
- signs and symptoms of recurrence, major bleeding and additional complications
- AMU and AEC contact details in event of complications and concerns
- Complete the PE Ambulatory proforma
- Arrange review in AEC within a week of discharge
- Refer to respiratory clinic
MONITORING ON WARD
- Daily clinical examination for signs of further embolism, right heart failure, and secondary infection of a pulmonary infarct
Monitoring enoxaparintreatment
- See Enoxaparin for VTE guideline
SCREENING
Screen for cancer
- In all patients with a confirmed PE, perform CXR, FBC, LFT, calcium and urinalysis
- Only offer further investigations for cancer to people with unprovoked PE if they have relevant symptoms or signs
Screen for thrombophilia
- If patient aged <45 yr with unprovoked PE, discuss screening for inherited or acquired thrombophilia with haematology consultant
DISCHARGE AND FOLLOW-UP
Duration of anticoagulation
- After a first provoked thromboembolic event, continue anticoagulation for 3 months and arrange follow-up in haematology and respiratory clinics for reassessment
- Continue indefinitely for life-threatening PE and refer to respiratory clinic
- For recurrent or unprovoked PE and minor provoked PE discuss with haematology and/or respiratory physician for extended anticoagulation before discharge and refer to respiratory clinic
- If patient has active cancer, reassess risks and benefits of continuing anticoagulation at 6 months in haematology, respiratory or oncology clinics
Outpatient investigations
- If evidence of right ventricular dysfunction or raised troponin or BNP biomarkers, arrange echocardiogram
- arrange follow-up for result in 10-12 weeks for respiratory clinic
- Refer all unprovoked PE patients to the local anticoagulation service and haematology clinic for further counselling and ongoing monitoring of anticoagulation
Advice to patient
- Many drugs (including alcohol) interact with warfarin or DOAC
- To remind their GP, if additional medication is added, that they are taking anticoagulant
- To inform dentist that they are anticoagulated
- Give advice on extended travel
- Provide PE information booklet
Women of childbearing age (pregnancy, pills, periods)
- Counsel that DOACs and warfarin may be harmful in pregnancy. Seek immediate advice if pregnant or trying to conceive
- Anticoagulation may lead to menorrhagia in 70% of women. Apixaban less commonly implicated than warfarin and rivaroxaban
- Do not stop contraception at time of PE diagnosis including combined oral contraceptive pill (COCP)
- refer patient to thrombosis clinic to discuss options
- anticoagulation negates ongoing thrombotic risk of the COCP. Stopping COCP may precipitate menorrhagia or lead to pregnancy whilst on a DOAC
Monitoring of warfarin
- Refer to anticoagulant management service for follow-up appointment date
- Give patient a completed yellow anticoagulation therapy record
- Ensure discharge letter includes diagnosis, dosage of warfarin and date of clinic appointment
- If anticoagulation to be monitored by GP, supply GP with written information (on separate sheet, stapled to discharge letter) about:
- indication for anticoagulation
- proposed duration of treatment
- proposed target range for INR
- details of anticoagulation in hospital (give dates, INR results and dosage taken)
Document
- Document in medical record
- patient has been given written and verbal information about warfarin and has been referred to anticoagulation clinic
- duration of treatment
- if definite risk factor identified
- outpatient investigations
- monitoring arrangements