RECOGNITION
- Stroke is a neurological deficit of sudden onset:
- with focal rather than global dysfunction
- with symptoms still present (if <24 hr) or lasting >24 hr, or resulting in death before 24 hr
- in which, after adequate investigation, symptoms are presumed to be of a non-traumatic vascular origin
- Treat all patients with symptoms, even if minor or improving, at time of assessment as a stroke
- only if symptoms have completely resolved within 24 hours, diagnose TIA
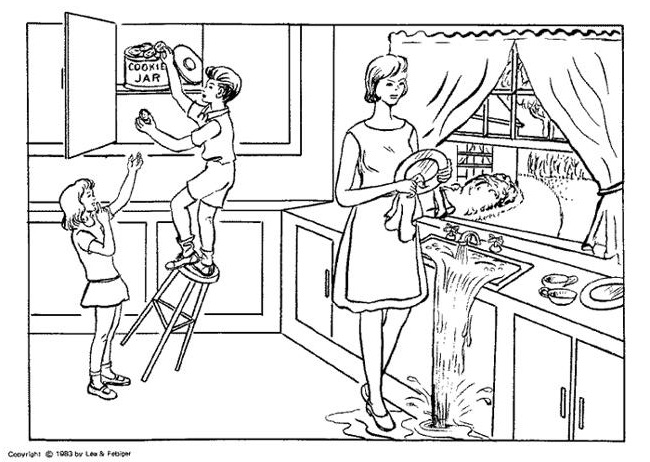
Symptoms and signs
Total anterior circulation syndrome (TACS)
- Involving both deep and superficial middle cerebral artery (MCA) territory
- New higher cerebral dysfunction (e.g. dysphasia, dyscalculia, visuospatial disorder) and homonymous visual field defect
- if consciousness is impaired and higher cerebral functions or visual fields cannot be tested formally, assume a deficit present
- Hemiparesis/hemisensory loss affecting at least 2 body areas (2 out of face, arm and leg)
Partial anterior circulation syndrome (PACS)
- More restricted cortical infarcts in the MCA territory, including isolated infarcts in the anterior cerebral artery (ACA) territory and striatocapsular infarctions
- Patients presenting with only 2 of the 3 components of the TACS or
- Motor/sensory deficit restricted to face or arm or leg
Lacunar syndrome (LACS)
- Small lacunar infarcts in the basal ganglia or pons
- Pure motor, pure sensory or sensori-motor deficit or
- Ataxic hemiparesis (with at least faciobrachial or brachiocrural involvement)
- acute focal movement disorders should probably also be included in this group
Posterior circulation syndrome (POCS)
- Infarcts in brainstem, cerebellum and/or occipital lobes
- Ipsilateral cranial nerve palsy with contralateral motor and/or sensory deficit
- Bilateral motor and/or sensory deficit
- Disorder of conjugate eye movement
- Cerebellar dysfunction without ipsilateral hemiparesis
- Isolated homonymous visual field defect
Causes of stroke
Ischaemic
- Large-artery atherosclerosis, small vessel atherosclerosis
- Cardioembolism, carotid/vertebral dissection
- Especially in younger patients, consider rarer causes:
- drugs, vasculitis, infection
- sickle cell disease, polycythaemia, haematological conditions
- sarcoidosis, metabolic disorder e.g. homocystinuria
Haemorrhagic
- Intracranial, subdural, and subarachnoid haemorrhage
Differential diagnosis
- Acute medical problem exacerbating effects of an older established stroke
- Seizures/Todd’s paralysis
- Migraine
- Functional
- Subarachnoid haemorrhage, extradural haemorrhage, subdural haemorrhage
- Space-occupying lesion
- Meningitis/encephalitis
- Metabolic (e.g. hypoglycaemia, hyponatraemia)
- Toxic (e.g. overdose)
- Anoxic encephalopathy (e.g. shock, arrhythmia)
- Trauma
IMMEDIATE ASSESSMENT
Ambulance service
- Pre-alert the stroke team with key patient details (name, date of birth, onset time, expected time of arrival, and contact number of ambulance crew)
Emergency department
- Take a detailed history (use telephone if necessary) to accurately ascertain onset time to determine appropriate hyper-acute treatments e.g. thrombolysis and thrombectomy
- Start hospital acute stroke pathway
Inpatient
- If an inpatient develops symptoms or signs raising strong suspicion of an acute stroke and onset time definite, arrange immediate CT head scan (plain) / CT angio and CT perfusion and inform stroke team immediately
Urgent investigations and actions
- Insert green venflon
- Glucose, U&E, FBC, INR, random cholesterol, LFT, CRP
- if patient on warfarin obtain INR urgently (use point of care device for immediate results)
- ECG (do not delay CT for this)
Immediate CT head scan plus
- If fit and independent, no contraindications to contrast, significant neurological deficit ( NIHSS >7) and within 4.5 hr of onset, ask imaging:
- if no signs of established infarction and no haemorrhage found on CT head scan, to perform CT angiogram (arch to Circle of Willis)
- If onset >4.5 hr or no known onset, also order CT perfusion scan
- If occlusion of a major intracerebral or extracerebral artery identified, discuss immediately with stroke consultant of the day
IMMEDIATE SPECIFIC MANAGEMENT
- Calculate NIHSS Stroke Scale (NIHSS)
- Contact research unit
Ischaemic stroke treatment
- Manage patients with antiphospholipid syndrome with an acute ischaemic stroke in the same way as patients with acute ischaemic stroke without antiphospholipid syndrome
Patient eligible for thrombolysis: within 4.5 hr of onset or small core and large penumbra
- Check contra-indications to IV thrombolysis
- e.g. post-operative, postpartum
- Unless contraindicated, start IV thrombolysis immediately
- use hospital acute stroke pathway
- In patients with contraindications to IV thrombolysis or with severe stroke (i.e. proximal MCA thrombus or basilar thrombus), consider thrombectomy
- arrange CT angiogram (Arch to circle of Willis) and CT perfusion
- In previously fit and independent patients within 4.5 hr of symptom onset or with a small core and large penumbra on the perfusion scan with occlusions in the CCA, ICA, M1, M2, ACA, basilar artery, or PCA, consider mechanical thrombectomy
- alert stroke nurse
- do not delay thrombolysis, mechanical thrombectomy can be arranged once treatment has been started
- In thrombolysed patients, do not give antiplatelets or anticoagulants for 24 hr
Patients not eligible for thrombolysis or thrombectomy
- Once CT head scan excludes haemorrhage, give aspirin 300 mg oral, rectal or via nasogastric tube immediately
- Transfer patient to acute stroke unit (ASU) as soon as possible within 4 hr of arrival.
- If urgent senior advice is required, call stroke consultant of the day
Intracranial haemorrhage treatment
Reverse anticoagulation
- Carry out point-of-care INR (if on warfarin), check full clotting screen and reverse immediately (within 3 hours)
- even with prosthetic valves
- Reverse anticoagulation with FXa inhibitors (rivaroxaban, apixaban, edoxaban, betrixaban) with Octaplex® or Beriplex® following discussion with on-call Haematologist
- Reverse anticoagulation with dabigatran using idarucizumab
- Reverse anticoagulation with warfarin immediately (within ≤3 hr)
- aiming for INR of 1.0 (even in patients with mechanical heart valves)
- give Vitamin K1 (phytomenadione) 5 mg IV immediately as slow bolus
- in patients with prosthetic valves and disabling cerebral infarct, stop warfarin and commence Aspirin 300mg once daily for one week immediately. Recommence warfarin after 1 week.
Other treatments
- Reduce systolic BP to ≤140 mmHg within one hour
- start GTN infusion at 1.5 mg/hr
- reassess and adjust dose every 5 min to a maximum 10.5 mg/hr. Follow ICH pathway
- If haemorrhage is subdural or subarachnoid, the stroke consultant may refer to neurosurgeons
- Call stroke nurse and start ICH Pathway
Acute venous stroke (cerebral sinus venous thrombosis)
- In patients with cerebral sinus venous thrombosis including those with secondary cerebral haemorrhage, start full dose anticoagulation
- initially unfractionated heparin, then warfarin aiming for target INR 2-3 unless contraindicated by other concurrent conditions
Stroke secondary to acute arterial dissection
- Refer to stroke team to decide between antiplatelets/anticoagulation
GENERAL MEASURES
- Admit to Stroke Unit
- Allow patient to sit up as tolerated (bed/chair) as soon as possible
- Mobilise conscious patients from day 1
- Ensure patients who are nil-by-mouth receive all necessary medication (use rectal, IV or nasogastric tube)
- Avoid sedatives (e.g. temazepam, chlorpromazine, haloperidol)
Hypoxia
- Check and clear airway. If oxygen saturation falls to <95% in spite of this, give supplemental oxygen. See Hypoxaemia guideline
Pyrexia (temperature >37.2°C)
- Look for source of infection and treat as indicated
- Treat pyrexia (temperature >37.5°C) with paracetamol 1 g oral or rectal 6-hrly
Hyperglycaemia
- Maintain blood glucose between 4-11 mmol/L. See Hyperglycaemia Triage guideline
Blood pressure
- Correct hypotension and try to prevent BP from falling
- Unless >220/120 mmHg or intracranial haemorrhage, do not lower BP acutely
- in intracranial haemorrhage, use GTN infusions and/or labetalol IV to lower blood pressure rapidly (within 1 hr) to ≤140/80 mmHg and maintain this level for 7 days
Statins
- If not already on a statin, start atorvastatin 80 mg/day (20 mg/day in the older frail person)
- Consider switching patients on simvastatin to atorvastatin
- less risk of adverse interactions
Prevention of DVT/pulmonary embolism
- Mobilise (out of bed) on day of admission
- Adequate hydration
- As soon as CT head scan has excluded intracerebral haemorrhage, start antiplatelet therapy
- For all patients not able to mobilise to the toilet independently, apply intermittent pneumatic compression (IPC) stockings day and night
- stop after first of 30 days or until mobile, or until discharged from acute care
- IPC may be removed temporarily during therapy, when mobilising, and while out of the ward for diagnostic tests
- Do not use compression stockings
- Do not use heparin/enoxoparin routinely (e.g. for age and stroke related immobility or infections alone)
- benefits in VTE prevention are counterbalanced by haemorrhagic complications with no evidence of an overall benefit on mortality and recovery
- Check calves for evidence of DVT at every ward round
- Stop VTE prevention at 30 days or at discharge, whatever comes earlier
Oral health
- Check and document oral hygiene during every ward round
- For patients who are nil-by-mouth, use chlorhexidine gluconate 1% dental gel or toothpaste for oral hygiene 12-hrly
- Keep dentures in during the day in all patients (unless very loose and safety risk)
Fluid and nutrition management
- Adequate and regular food and hydration
- Patients who are nil-by-mouth, start on nasogastric feeding as soon as possible within 24 hr
- In all patients receiving palliative care, give comfort feeding and oral fluids as desired and tolerated
Assess swallowing at bedside
- Check patient is:
- alert and co-operative
- able to sit up for feeding
- able to cough on demand
- not drooling excessively
- Sit patient up, listen to voice and give 5 mL of water on a spoon
- Watch and feel swallow with fingers on larynx
- Observe for 2 min, looking for:
- choking or impaired breathing
- delayed swallow
- cough
- change of voice
- If 5 mL swallowed without difficulty, give 50 mL of water before giving soft diet
- If there is any doubt about swallowing, recommend nil-by-mouth
- give fluid IV/SC. See Fluid maintenance guideline
- ask speech therapist or stroke team to assess swallowing
Fluids
- Unless patient in urinary retention, do not catheterise
- In patients who are nil-by-mouth, dehydrated or at risk of dehydration, follow IV Fluid maintenance guideline
Nasogastric tube feeding
- In patients with severe stroke and dysphagia, start nasogastric feeding within 24 hr (unless expected to die within hours)
- Prescribe metoclopramide 10 mg 8-hrly (5 mg if <50 kg body weight) via nasogastric tube for 3 weeks or until nasogastric feeding no longer required (whichever occurs earlier)
- In mild strokes, where normal swallow expected to return, review after 48 hr
- if dysphagia still present, pass nasogastric tube
- Where a standard nasogastric tube cannot be kept in place safely and reliably, consider a nasal bridle
- Refer patients with persistent dysphagia after 3 days for dietary advice
- consider further investigation (e.g. video fluoroscopy)
PEG (percutaneous endoscopic gastrostomy)
- If NG tube not tolerated and patient unable to take sufficient nasogastric/oral diet for 3 or more days, refer urgently for PEG
- If nasogastric feeding successful but no significant recovery of swallowing occurs, consider referral for PEG within 4 weeks
- If there is some recovery of swallowing and nasogastric feeding successful, PEG referral may not be necessary
- continue nasogastric feeding until patient able to eat normally
Fracture prevention
- If stroke patient likely to remain housebound, or discharged to a care facility, prescribe calcium and vitamin D
Nicotine withdrawal
- Offer nicotine patches to all smokers, unless they do not intend to stop smoking or if they have contraindication
COMPLICATIONS
Malignant MCA syndrome
- If deterioration of consciousness within first 48 hr in patients with large MCA territory infarcts ( NIHSS score >15 with item 1a ≥1 (e.g. drowsy patient)), consider malignant MCA syndrome
- Arrange urgent CT head scan and discuss with stroke consultant of the day
Result of CT scan
- An infarct affecting at least 50% of the middle cerebral artery territory with or without additional infarction in the territory of the anterior or posterior cerebral artery on the same side, or with an infarct volume of >145 cm3 confirms the diagnosis
Treatment
- Increase neurological observations to every 15 min
- Consider referring urgently to neurosurgery (within 24 hr of stroke onset) to allow surgery within 48 hr
- do not wait for midline shift on head CT scan or abnormal pupillary responses
- in potential candidates for hemicraniectomy, avoid mannitol or hypertonic saline (may mask signs of deterioration and delay surgery)
Stroke progression
- Treat as an emergency
- Confirm by repeating NIHSS Score
- increase of ≥4 points indicates clinically significant deterioration
- Repeat head CT scan and seek senior advice
- Review differential diagnosis
- Consider MR, EEG (for possible encephalitis or epilepsy), lumbar puncture
Infarct progression/further stroke
- Highest risk in minor strokes/TIAs
- check aspirin 300 mg oral or rectum started
- Consider haemorrhagic conversion especially in large infarcts or in thrombolysed patients
Intracerebral haemorrhage progression
- If deterioration in neurological signs/level of consciousness after admission, re-scan immediately
- unless there are good reasons not to consider surgery, refer to neurosurgeons for advice
- recheck INR and correct
Other causes
- Cerebral emboli, or vasculitis
- Hydrocephalus especially in cerebellar strokes or in patients with intracerebral haemorrhage
- refer previously fit patients to neurosurgery
Pneumonia after starting oral fluids
- Reassess swallowing, treat as Hospital-acquired pneumonia unless diagnosed on admission
Urinary retention
- Relieve by in and out catheter, record drained volume
- Monitor bladder volume by bladder scan
- intermittent catheterisation as needed
- Check for faecal impaction and treat
- If retention recurrent, start tamsulosin MR 400 microgram/day
- do not use in patients where BP lowering effect could be a problem
- for patients with nasogastric tube in situ, use doxazosin 1 mg once a day, increased as necessary to maximum 16g/day which may be crushed (unlicensed)
- Avoid indwelling catheter
DVT/pulmonary embolism
- If CT head scan has excluded haemorrhage, treat. See Deep venous thrombosis and Pulmonary embolism guidelines
- In patients with haemorrhagic stroke and symptomatic DVT/PE, discuss anticoagulation or placement of a caval filter to prevent (further) PE with stroke consultant
Shoulder pain
- Prevent by not pulling on the affected arm and always supporting its weight
- Maintain correct position and adequate support, consult physiotherapist, consider paracetamol
- For subluxation, consider functional electrical stimulation
- If pain persists, consider addition of NSAIDs, supraspinal nerve block, TENS or intra-articular corticosteroids
Depression
- Treat conventionally
Seizures
- Treat conventionally
Pressure sores
- Treat diarrhoea effectively, prevent hypotension, ensure adequate nutrition, check that pressure relief adequate. Involve tissue viability team
FURTHER INVESTIGATIONS
General
- If random glucose >7.5 mmol/L, request fasting glucose and HbA1c
- Lipid status (<48 hr after stroke or after 6 weeks)
- Chest X-ray
For specific indications
Cardiac murmurs and/or history of rheumatic fever and/or no risk factors for atheroma
- Consider echocardiography to exclude a cardiac source of embolism
Patients (age <55 yr) with no vascular risk factors nor cardiac/arterial sources of embolism
- Request bubble contrast echocardiogram to exclude atrial septal defect (ASD)/patent foramen ovale (PFO)
- if positive for ASD/PFO, no other cause for the stroke identified (cryptogenic), and aged <55 yr, refer to cardiology for consideration of closure
In patients with no risk factors for atheroma
- Screen for arteritis (CRP, ANA, ANCA, Rh Factor)
Young patients with no atherosclerosis/risk factors
- Investigate for thrombophilia
- FBC: exclude polycythaemia, thrombocytosis, sickle cell disease
- lupus anticoagulant, anticardiolipin antibodies
- JAK-2 mutation studies: to exclude myeloproliferative disorders
- fasting homocysteine levels
Patent Foramen Ovale (PFO) or venous thrombosis (concurrent PE, cerebral sinus thrombosis)
- Check protein C, protein S, Factor V Leiden and PT gene mutation
- discuss with haematologist
- send sample which will be frozen and stored in the lab (for 6 months)
Patients age <55 yr or those without vascular risk factors
- Consider CT or MR angiography to exclude dissection
Patients without vascular risk factors where the diagnosis is in doubt
- Consider MR (DWI) scan of brain with ADC mapping to confirm an infarct/show potential alternative pathology, or demonstrate normality
- discuss with neuro-radiologists for protocol
- If several repeated scans considered necessary to exclude recurrent silent ischaemic events, consider MR scan in preference to CT to reduce radiation exposure
SUBSEQUENT MANAGEMENT
Rehabilitation
- Start active rehabilitation on day 1
- unless consciousness impaired, sit out and mobilise from day 1
- Full multidisciplinary assessment to identify rehabilitation goals
- nurses, occupational therapist, physiotherapist, doctors, speech and language therapist, clinical psychologist
- involve dietitian, social worker, pharmacist, other medical or surgical specialties as necessary
Quick recovery
- If patient recovers rapidly and is left with no significant residual disability after a few days, arrange for urgent carotid Doppler (within 1 working day)
- make sure secondary prevention (see below) is in place
- 12% of patients with minor strokes will extend or have a further stroke within 1 week
Secondary prevention
- Advise to stop smoking
- Give dietary advice. Reduce salt intake
- Advise to exercise regularly. Brisk walking for 30 min
- Identify and treat diabetes. Keep HbA1c below 53 mmol/mol
Antiplatelet treatment
- Give patients with TIA or minor non-disabling stroke, clopidogrel 300mg STAT or Aspirin 300mg STAT then Clopidogrel 75mg once daily plus Aspirin 75mg once daily for 21 days with PPI cover for 21 days with Lansoprazole 30mg once daily
- after 21 days, stop aspirin and continue clopidogrel 75mg once daily monotherapy indefinitely
- In established stroke, once haemorrhage excluded by CT, unless contraindicated, aspirin 300 mg/day for 2 weeks or until discharge
- in patients with history of dyspepsia, add proton pump inhibitor
- after 2 weeks, or at discharge, change to clopidogrel 75 mg/day indefinitely
- In patients allergic to, or genuinely intolerant of aspirin, use clopidogrel 300 mg STAT followed by 75 mg once daily
- if allergic to both aspirin and clopidogrel, give dipyridamole MR 200 mg 12-hrly
Anticoagulation
- In all patients with atrial fibrillation/flutter (AF) who have no contraindications, commence anticoagulation with a direct oral anticoagulant (DOAC) or warfarin
- in mild non-disabling stroke, start anticoagulation between day 2 and day 14
- in severe disabling stroke, delay start of anticoagulation to 14 days or longer
- Refer patients with AF, a CHAD2DS2-VASc score ≥1, and contraindication to anticoagulation to cardiology for consideration of atrial appendage closure
Other medication
- Give atorvastatin 20 mg at night once a day (start low uptitrate to 80 mg where tolerated)
- check levels after 3 months and adjust dose to reduce non-LDL cholesterol by 40%
- review annually
- Unless there is an important reason to continue (e.g. premature ovarian failure, severe menopausal symptoms), stop contraceptive pill/hormone replacement therapy
- in premenopausal women, provide advice on alternative methods of contraception
- Reduce blood pressure to a target of ≤130/80 mmHg starting within 24 hr of minor stroke/TIA and within 2 weeks of moderate to severe stroke, in line with current British Society of Hypertension guidelines
DISCHARGE
- The acute stroke unit provides information packs for patients and carers
- assist in discharge planning and arrangements for continued outpatient rehabilitation
- contact the stroke family support worker where needed
Follow-up
- Follow-up at 6 weeks, 6 months, and annually
- arrange first follow-up in a specialist hospital clinic
- further follow-ups can be carried out by stroke-trained teams in the community
Referrals
- Refer patients aged ≤55 yr to the young stroke clinic for follow-up
- Refer all patients on anticoagulation to the anticoagulation follow-up clinic
- Refer smokers to smoking cessation services
- Assess functional status (Rankin), continence, pain, mood, cognition, and barriers to return to work, leisure activities and driving in clinic and refer as appropriate
- Consider referral to the early supported discharge team
- Consider and record whether a joint care plan with social services is required
Discharge summary
- Diagnosis including OCSP class and NIHSS at admission
- Thrombolysed/not thrombolysed
- NIHSS on discharge, level of dependence, mobility
- Risk factor assessment with instructions for secondary prevention
- Driving advice
- Details of any clinical trial patient taking part in
Patient and relatives
- Give patient a copy of the discharge summary
- Ensure patient and relatives are aware of diagnosis, discharge date, follow-up arrangements and secondary prevention measures
Driving
- Check for hemianopia and hemi-inattention in all drivers
- not always obvious to patient and disqualifies from driving until resolved
- Give driving instructions verbally and in writing
- do not drive for 1 month and inform insurance of stroke
- if back to normal within 1 month and no recurrence, patient may drive again
- if persistent deficit or recurrence, patient must inform DVLA and await assessment by a doctor