SPECIFIC CONDITIONS
If patient has any of the following conditions, follow appropriate condition-specific guideline
- For neutropenic sepsis in cancer patients – see Neutropenic sepsis guideline
- For sepsis management in children – see Paediatric guidelines
- For peri-natal sepsis – see Obstetric and Neonatal guidelines
DEFINITIONS
- Sepsis – a life-threatening organ dysfunction due to dysregulated host response caused by an infection. It is a medical emergency
- Septic shock is associated with a higher risk of mortality (>40%) and refers to patients with sepsis who:
- remain hypotensive despite adequate fluid resuscitation and require vasopressors to maintain a mean arterial pressure (MAP) ≥65 mmHg
- have persistently elevated serum lactate (≥2 mmol/L)
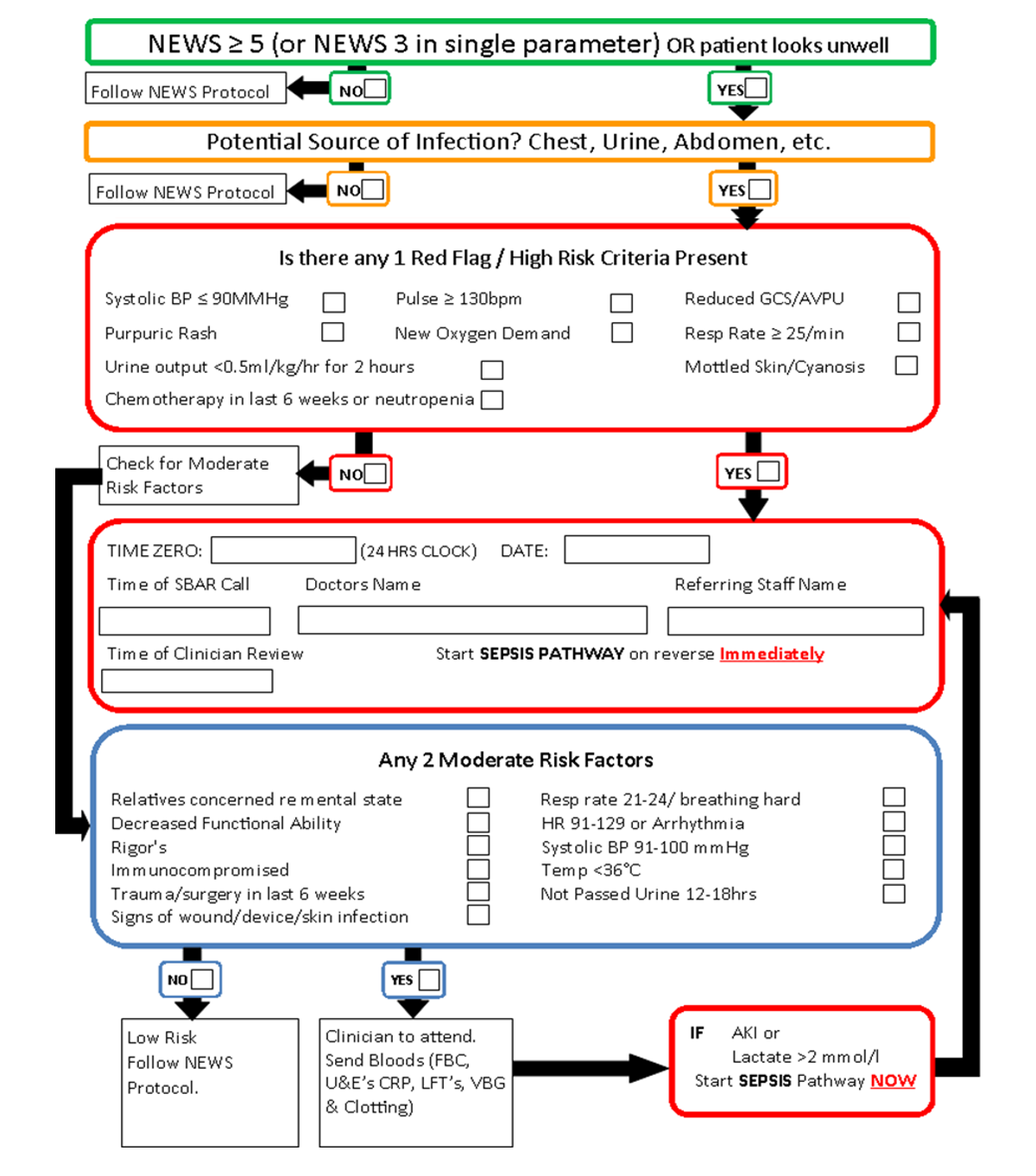
SCREENING
- All patients who have a NEWS ≥5 (or) any individual NEWS element ≥3, screen for sepsis by completing Sepsis Proforma Looking for red flags and moderate risk factors
IMMEDIATE MANAGEMENT
- Start Sepsis Six if the patient satisfies 1 of the following:
- presence of 1 red flag sign or
- presence of 2 moderate risk factors along with AKI and/or lactate ≥2
Sepsis Six
- Complete all actions in one hour
- Ensure senior clinician attends
- Administer Oxygen
- Obtain IV access
- Take blood cultures, glucose, lactate, FBC, U&Es, CRP and clotting
- Consider cultures from potential sources of infection & Chest X-ray
- if probable CNS infection, perform lumbar puncture. See Lumbar puncture
- Give IV antimicrobials
- Give IV fluids
- see Adult fluid management guideline
Monitor
- NEWS2. See NEWS
- Measure urine output
- may require urinary catheter
- start fluid balance chart & complete hrly
- Check serial lactates
- corroborate high VBG lactate with arterial sample
- If lactate >4mmol/L, call critical care
- Record observations at least every hour
- if initial lactate raised or if clinical condition deteriorates, at least every 30 minutes
Antimicrobials
Penicillin Allergy
- True penicillin allergy is rare
- Ask the patient and record what happened when they were given penicillin
- If any doubt about whether patient is truly allergic to penicillin, seek advice from a microbiologist or consultant in infectious diseases
Only accept penicillin allergy as genuine hypersensitivity if convincing history of either rash within 72 hr of dose or anaphylactic reaction
Infection Control alerts
- Check for IC alert
- if IC alert not available, check previous 12 months of microbiology reports
- If MRSA present, treat as tagged for MRSA. See MRSA management
- high risk of MRSA: recent history of MRSA, patient in other hospital/nursing home in last 12 months, sepsis likely to be hospital-acquired, or line infection suspected
- If ESBL, MGNB, CARB present, treat as tagged for ESBL. See ESBL/MGNB/CARB management
- ESBL or MGNB tag: history of ESBL-producing or multi-resistant Gram-negative Bacilli
Choice of anti-microbials
Select type of patient from list:
- First line: Meropenem 0.5-1 g IV 8-hrly plus vancomycin IV by infusion – see Vancomycin guideline
- Alternative (true penicillin allergy): Meropenem 0.5-1 g IV 8-hrly plus vancomycin IV by infusion – see Vancomycin guideline. If anaphylaxis to penicillin, discuss with consultant in infectious diseases or microbiologist
- First line: Piperacillin/tazobactam 4.5g IV infusion 8-hrly plus vancomycin IV by infusion – see Vancomycin guideline
- Alternative (true penicillin allergy): Aztreonam 2g IV 6-8-hrly plus vancomycin IV by infusion – see Vancomycin guideline
- First line: Meropenem 0.5-1g IV 8-hrly alone
- Alternative (true penicillin allergy): Meropenem 0.5–1 g IV 8-hrly alone. If anaphylaxis to penicillin, discuss with consultant in infectious diseases or microbiologist
- First line: Piperacillin/tazobactam 4.5 g IV infusion 8-hrly (if necessary, increase to 4.5g IV 6-hrly; increased frequency may be used for severe infections)
- Alternative (true penicillin allergy): Aztreonam 2g IV 6-8-hrly plus vancomycin IV by infusion - see Vancomycin guideline
Septic shock
- Consider patient in septic shock if any of the following are present despite 30 mL/kg of fluid resuscitation within first 3 hr
- mean arterial blood pressure ≤65 mmHg or
- serum lactate persistently elevated ≥2 mmol/L on repeated measurements
- Consider immediate escalation to senior clinician (registrar and above) and/or to critical care team
- Once decision is made, admit patients requiring critical care to the ICU within 6 hours
CODING FOR DIAGNOSIS OF SEPSIS
- Correct coding of sepsis enables local and national data to accurately reflect the incidence of sepsis
- Current consensus definition is 'organ dysfunction' and dysregulated host response secondary to an infectious source
- Do not document localised infections (non-septic infections) in medical record as sepsis (e.g. terms like urosepsis, biliary sepsis, chest sepsis etc., may be inaccurately coded as systemic sepsis)
- good practice is for a responsible consultant to confirm that initial diagnosis of sepsis is a 'true sepsis' or indicate only a localised infection present (rather than generalised sepsis), code as a localised infection only or a 'non-septic infection'
Last reviewed: 2023-10-23