RECOGNITION AND ASSESSMENT
Symptoms and signs
- Unusual unless calcium (Ca2+) >3.0 mmol/L
- GI: nausea, vomiting, constipation, abdominal pain
- Renal: polyuria, polydipsia
- CVS: hypertension, on ECG: altered QT interval, long PR, wide QRS, arrhythmias
- CNS: various including depression, cognitive difficulties, headache, altered consciousness, acute psychosis
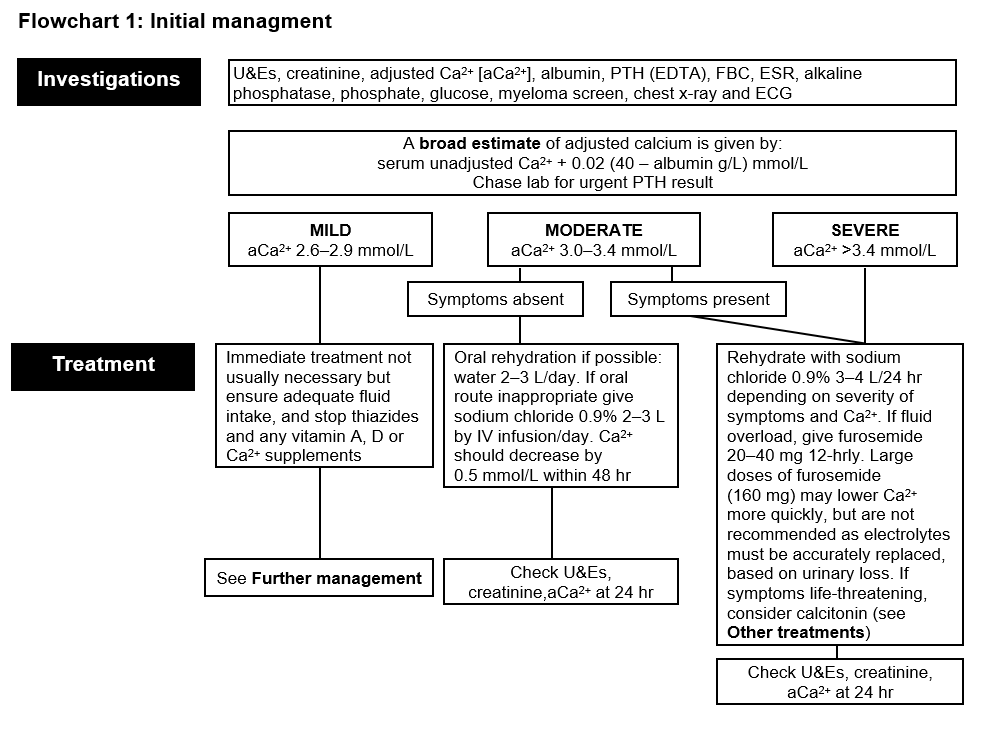
Investigations
- Adjusted Ca2+ [aCa2+], albumin, PTH (EDTA), alkaline phosphatase, phosphate
- A broad estimate of adjusted calcium is given by: serum unadjusted Ca2+ + 0.02 (40 - albumin g/L) mmol/L
- Chase lab for urgent PTH result
- U&Es, creatinine, glucose, myeloma screen
- FBC, ESR
- Chest x-ray and ECG
INITIAL MANAGEMENT
- Reduce aCa2+
- Stop thiazides and any vitamin A, D or Ca2+ supplements
- For guidance follow Initial management and then Response to treatment flowcharts
- Treat the underlying cause.
MANAGEMENT OF CAUSE
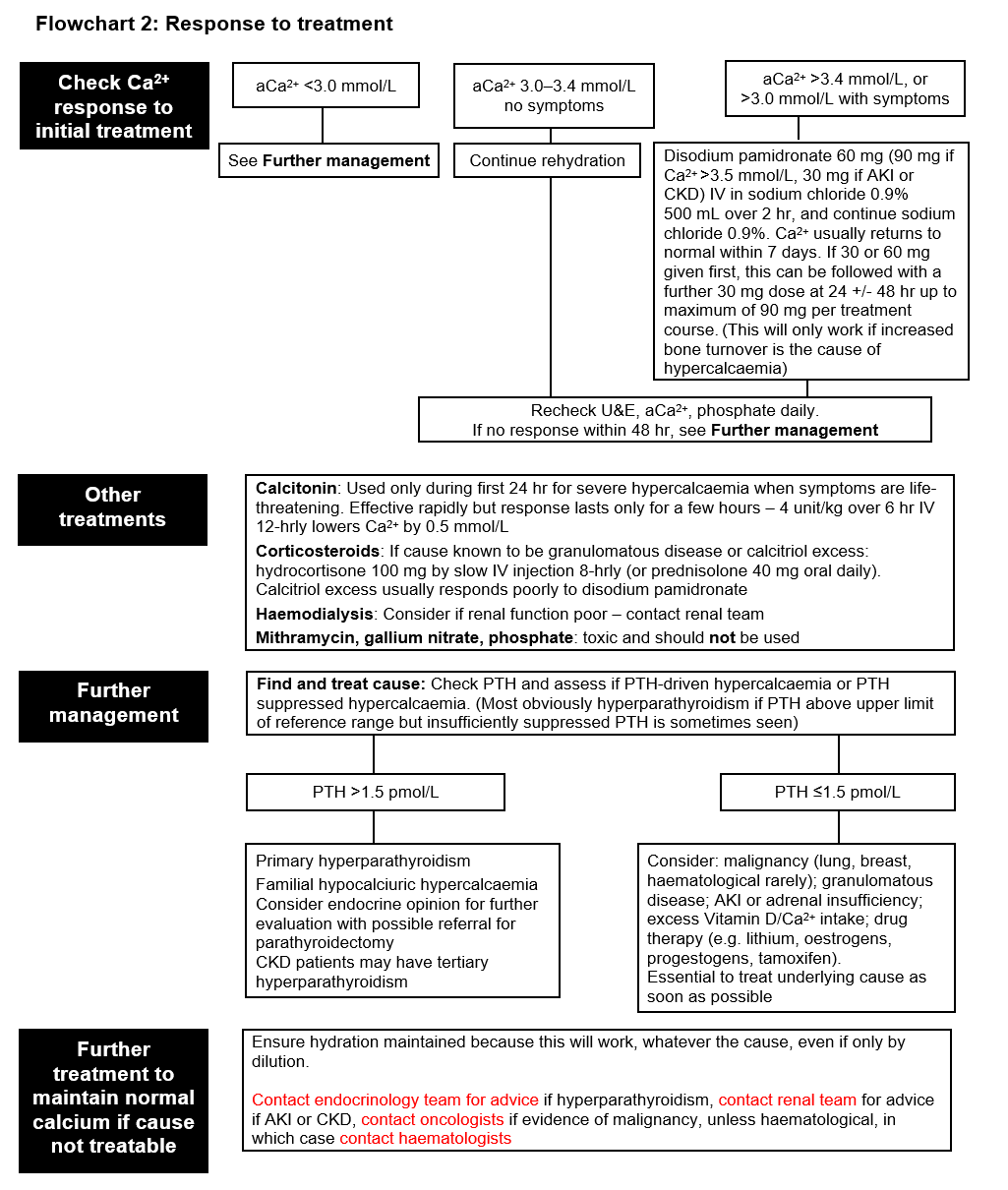
- Check PTH and assess if PTH-driven hypercalcaemia or PTH-suppressed hypercalcaemia. (Most obviously hyperparathyroidism if PTH above upper limit of reference range but insufficiently suppressed PTH is sometimes seen)
- If PTH >1.5 pmol/L, consider Primary hyperparathyroidism or Familial hypocalciuric hypercalcaemia. CKD patients may have tertiary hyperparathyroidism
- Contact endocrinology team for advice if hyperparathyroidism. Contact renal team for advice if AKI or CKD
- If PTH ≤1.5 pmol/L, consider: malignancy (lung, breast, haematological rarely); granulomatous disease; AKI or adrenal insufficiency; excess Vitamin D/Ca2+ intake; drug therapy (e.g. lithium, oestrogens, progestogens, tamoxifen).
- Contact oncologists if evidence of malignancy, unless haematological, in which case contact haematologists
- If treatable, treat underlying cause as soon as possible
- If cause not treatable, ensure hydration maintained because this will work, whatever the cause, even if only by dilution
Last reviewed: 2024-02-12